COVID-19 is a highly transmissible disease that has spread rapidly worldwide. It was first detected in Wuhan, China, in December 2019 and was subsequently declared a pandemic by the World Health Organization on March 11, 2020. According to Li et al. (2023), on April 6, 2023, there had been 762,201,169 reported COVID-19 cases globally, and despite companies developing safe and effective vaccines and governments disseminating these, the number of new cases and fatalities remains high, with 6,893,190 deaths reported as of April 6, 2023.
Despite the availability of a safe COVID-19 vaccine, a major challenge is people’s reluctance to use it. For example, only 58% of German parents intend to utilize the COVID-19 vaccine (Brandstetter et al., 2021), while in Russia, 40% of people declined receiving COVID-19 immunization (Lazarus et al., 2021). Pakistan’s vaccination rate is also low, with only 66% willing to be vaccinated as of July 2021 (Ahmad Kamboh et al., 2022). This low rate compromises vaccine effectiveness, endangers lives, and increases the likelihood of new COVID-19 variants forming (Dhama et al., 2021). Thus, this study examined how religiosity and knowledge of the COVID-19 vaccine impact people’s intention to get vaccinated.
In this study, religiosity refers to belief in God and commitment to act according to God’s principles. People with religious beliefs view everything around them as subject to God’s commandments and act according to their religious teachings. Previous research has shown that religious beliefs influence attitudes and behaviors, including the intention to consume pharmaceutical products (Kasri et al., 2023) and vaccines against various diseases (Grabenstein, 2013). However, Trepanowski and Drążkowski (2022) found no relationship between Muslims’ religious beliefs and COVID-19 vaccination uptake. Therefore, there is a need for empirical evidence on the impact of religious beliefs on COVID-19 vaccine usage intention.
The world has produced safe and effective vaccines for COVID-19 (Zheng et al., 2022), but sometimes, religious beliefs can influence people’s medical decisions (Garcia & Yap, 2021). Individuals with strong religious beliefs may prioritize prayers over medicine, believing that diseases result from evil and that divine intervention is the only cure. For example, Bishop Gleen remarked in a US sermon in his church that he “firmly believe[s] that God is larger than this dreaded virus” and “people are healed” (Bok et al., 2021, p. 2). Similarly, one attendee at a Muslim religious event in Malaysia stated, “None of us have a fear of Coronavirus. We are afraid of God” (Dein et al., 2020, p. 3). Some people with strong religious beliefs oppose using scientific methods (e.g., medicine or vaccines) instead of religious methods (Trepanowski & Drążkowski, 2022). In Pakistan, a Muslim-majority country, we have heard that some believe the COVID-19 vaccine contains nonhalal animal derivatives, like pork, which Islam prohibits. Thus, people’s religious views and willingness to be vaccinated influence the effectiveness of vaccination campaigns (Hossain et al., 2021). According to the above literature, we proposed the following hypothesis:
Hypothesis 1: Religious belief will be negatively related to intention to be vaccinated against COVID-19.
Research has highlighted the importance of people’s knowledge about and attitude toward the COVID-19 vaccine (Hossain et al., 2021; Mohamed et al., 2021). Knowledge about the COVID-19 vaccine refers to people’s understanding of the information available about the COVID-19 vaccine, such as its efficacy, effectiveness, and development (Mohamed et al., 2021). Individuals with a good understanding of COVID-19 vaccines are less hesitant to receive the vaccine (Hamdan et al., 2021), whereas a lack of knowledge can hinder the effectiveness of an immunization campaign (Garcia & Yap, 2021). Informed individuals tend to be health-conscious, aware of potential vaccine risks and benefits (Zheng et al., 2022), and less susceptible to antivaccine campaigns (Dhama et al., 2021). Therefore, we proposed the following hypotheses:
Hypothesis 2: Knowledge about COVID-19 vaccines will be positively related to intention to get vaccinated.
Hypothesis 3: Knowledge regarding COVID-19 vaccination will moderate the influence of religiosity on intention to receive the COVID-19 vaccine, resulting in a less negative relationship for those with high levels of knowledge and a more negative relationship for those with low levels of knowledge.
Method
Participants and Procedure
This study surveyed undergraduate and postgraduate students from public sector colleges in Balochistan, Pakistan, using a convenience sampling approach and a self-administered survey. Of 350 questionnaires we distributed, 277 were returned, representing an initial response rate of 79.14%. After removing cases with more than 15% missing values (seven responses) and responses with suspicious patterns (19 cases), 251 cases were used for analysis. Of these, 137 (54.58%) were from women and 114 (45.6%) were from men. The mean age was 23.4 years (range = 18–30). We obtained informed consent from all individual participants included in the study.
Measures
The study used established measures scored on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). We measured intention to use a COVID-19 vaccine with the four-item scale from Wong et al. (2020). A sample item is “I intend to get vaccinated against COVID-19.” We measured religiosity using an eight-item scale adopted from Wang et al. (2021). A sample item is “What my religion offers me the most is comfort in times of trouble and sorrow.” Finally, we assessed knowledge of the COVID-19 vaccine using a 10-item test designed and validated by Mohamed et al. (2021). A sample item is “The vaccine protects the receiver from getting COVID-19.”
Results
Descriptive Statistics
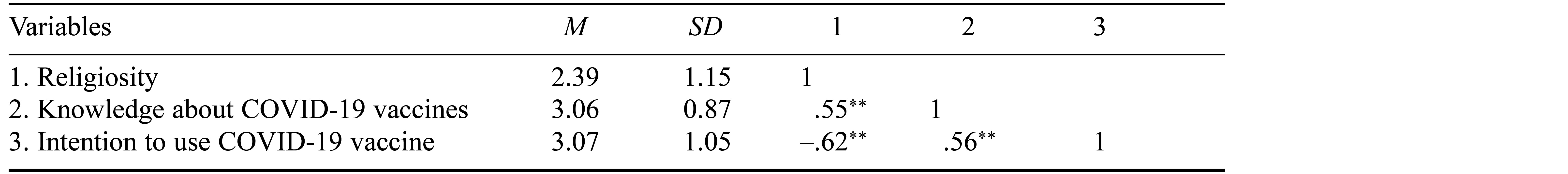
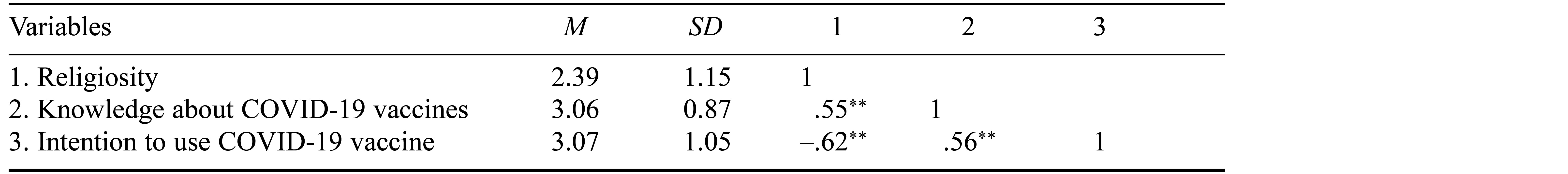
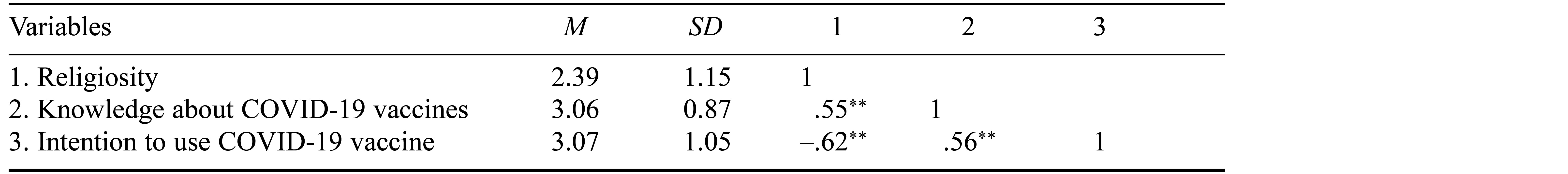
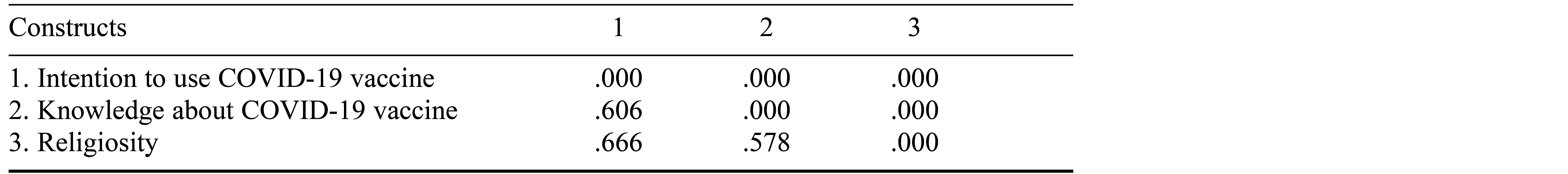
Descriptive statistical analysis was conducted using SPSS 24.0. Table 1 presents the means, standard deviations, and correlations among the study variables. The results indicated that religiosity had a negative correlation with the intention to get the COVID-19 vaccine and a positive correlation with knowledge about the COVID-19 vaccine.
Table 1. Descriptive Statistics
We used partial least squares structural equation modeling (PLS-SEM), a multivariate variance-based data analysis tool, to evaluate the study’s complex and prediction-oriented model. We utilized SmartPLS software for this investigation. The research model was assessed in two stages: first, we examined the measurement model; second, we examined the structural model. Before the model assessment, we checked for common method bias using variance inflation factors, and the values were lower than the threshold of 3.3, ruling out the presence of any common method bias in this study (Kock, 2015).
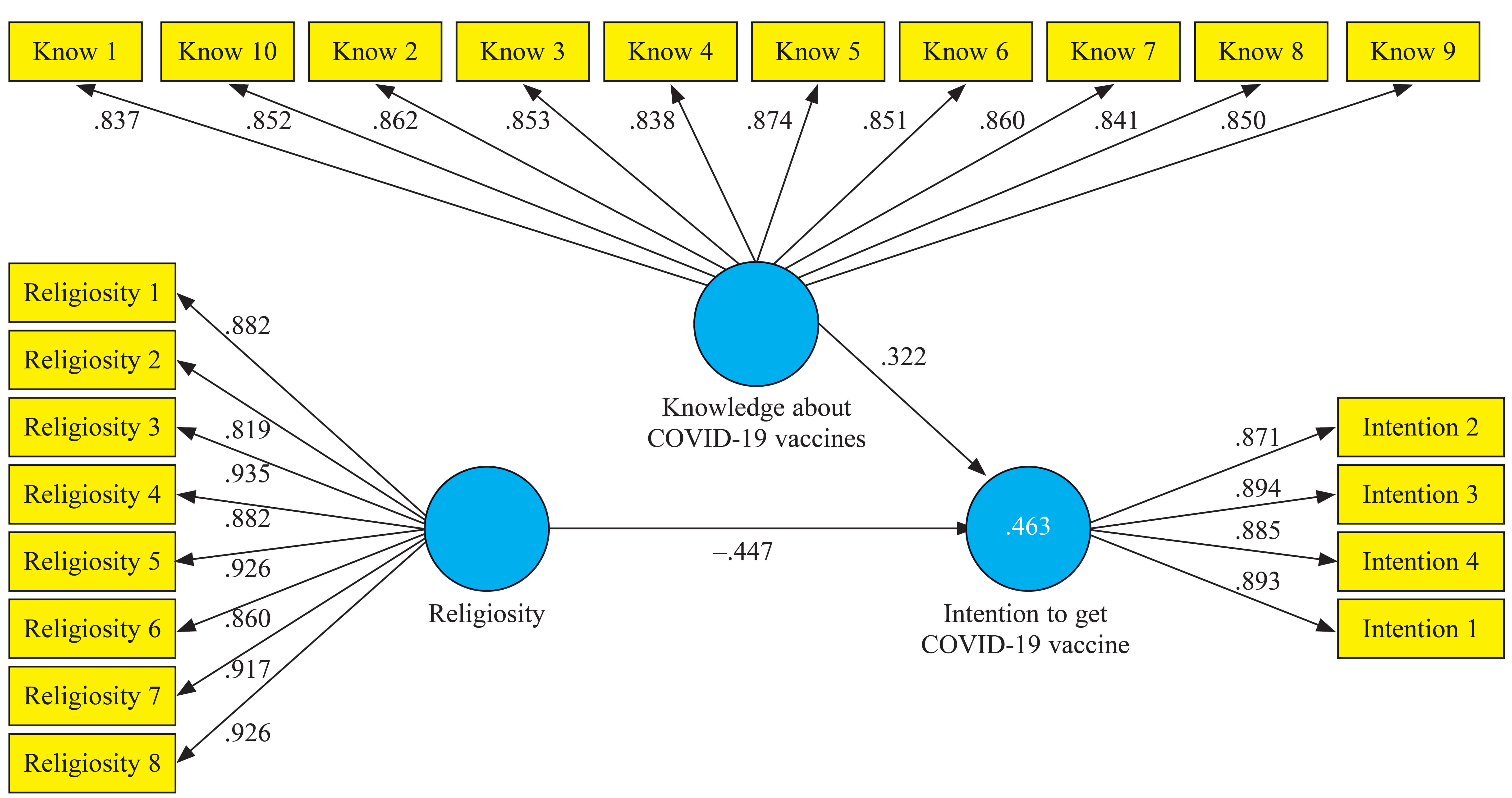
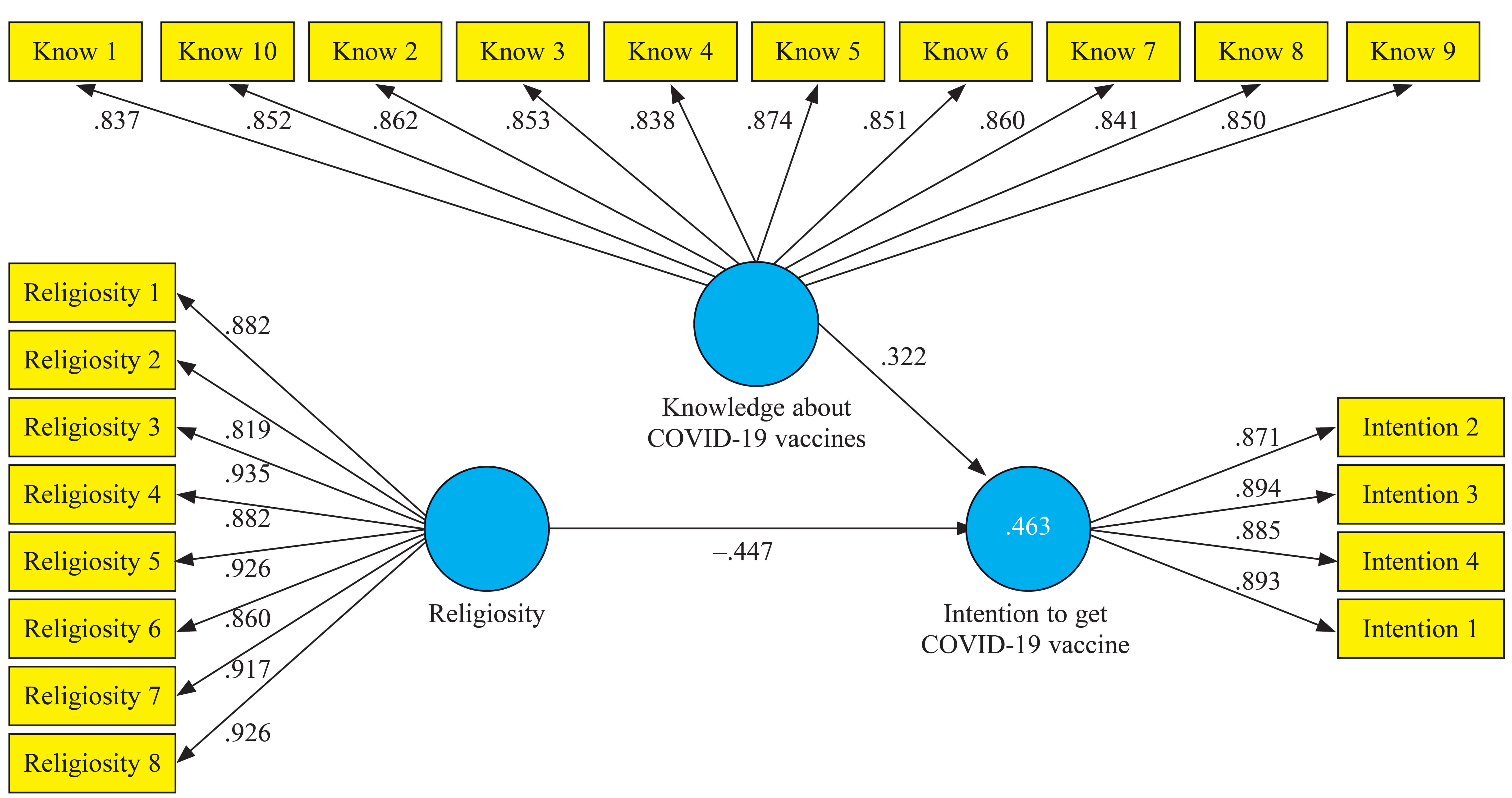
Measurement Model Assessment
In the measurement model assessment, as shown in Figure 1, we evaluated observable indicators’ reliability and validity by examining their relationship with latent variables (Hair et al., 2022). We used factor loadings to assess observable indicators’ reliability, with values of ≥ .70 indicating acceptable reliability. In this study the factor loadings ranged from .819 to .935, indicating good reliability. Cronbach’s alpha values for all variables (religiosity = .964, knowledge = .958, intention = .908) exceeded the minimum threshold of .70, indicating acceptable internal consistency reliability (Hair et al., 2022).
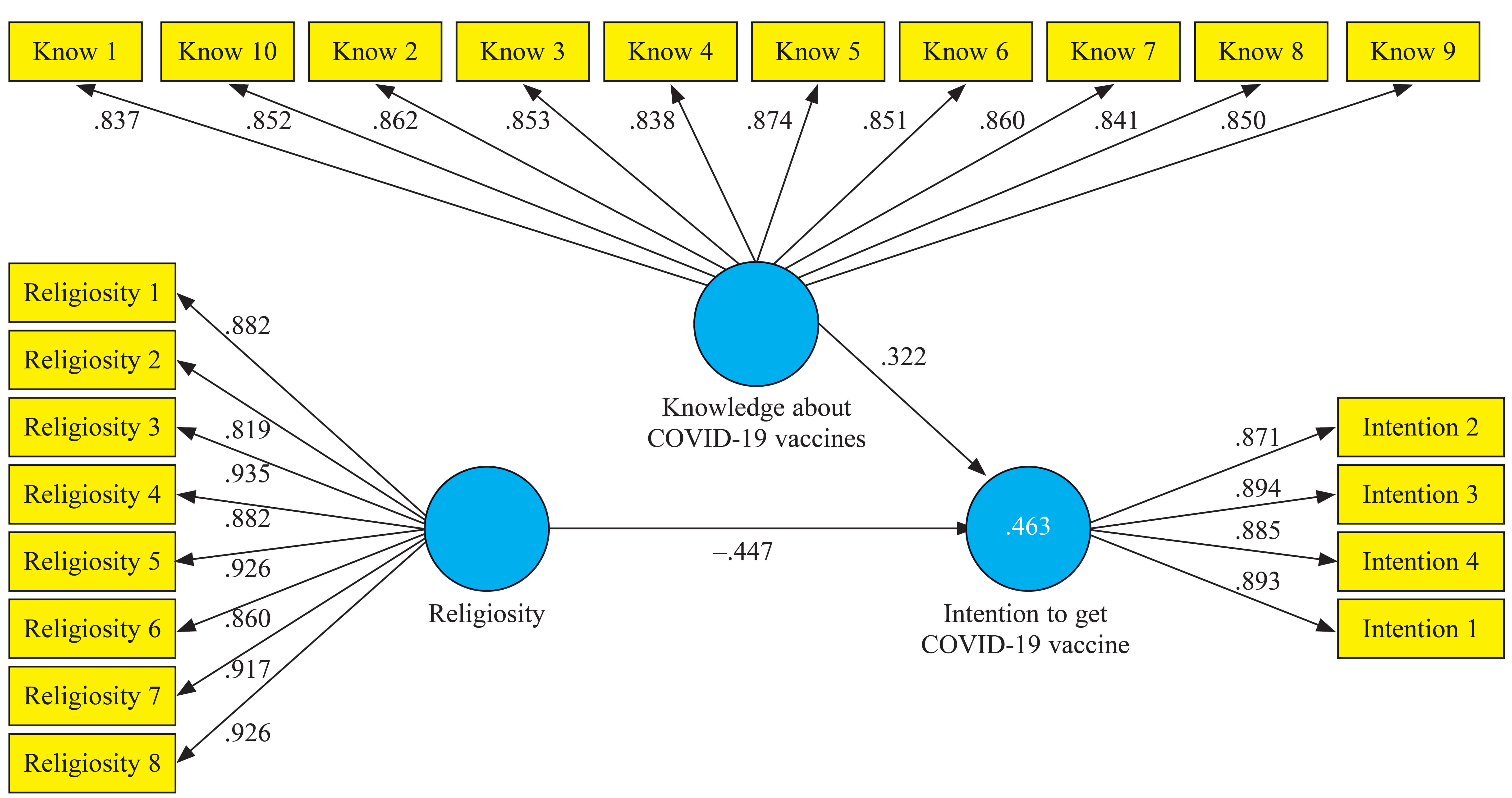
Figure 1. Measurement Model
Note. Observable indicators are shown in yellow; constructs are shown in blue; the values between yellow boxes and constructs are factor loadings. Know = knowledge.
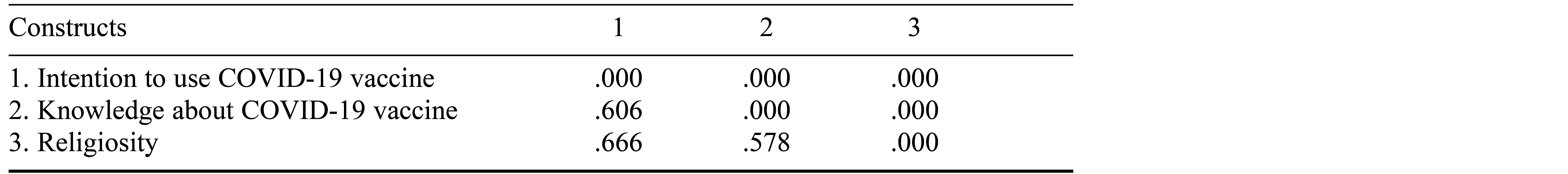
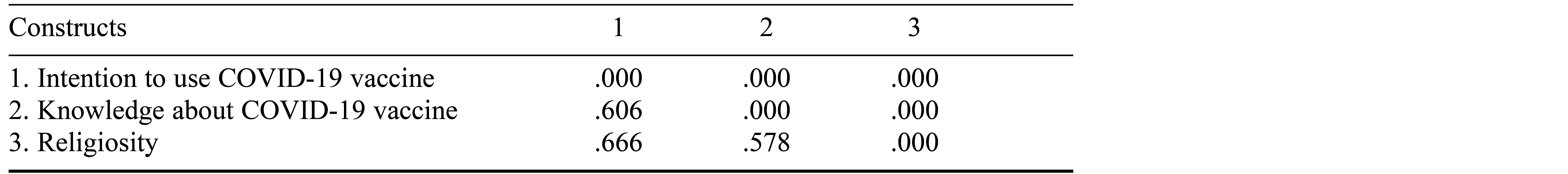
We estimated the convergent validity of constructs using average variance extracted, and the values were greater than .50 (range = .772 to .799), thus retaining convergent validity (Hair et al., 2022). We used the Heterotrait-Monotrait ratio of correlations to compute discriminant validity. A construct is considered to have good discriminant validity if the values of Heterotrait-Monotrait constructs are below .90 (Henseler et al., 2015). The study’s findings (see Table 2) reveal that values were less than .90, thus affirming the discriminant validity.
Table 2. Heterotrait-Monotrait Ratio (HTMT)
Structural Model
The structural model depicts the hypothesized links between the study’s latent variables. We evaluated the model fit by calculating standardized root mean square residual (SRMR), which is an adequate measure of model fit in PLS-SEM research (Henseler et al., 2015). A model is considered to have a good level of fit if SRMR < .08. The current study’s SRMR score was .044, indicating a well-fitting model.
We further analyzed the model fit by calculating R2, f2, and Q2 values. R2 denotes the power of external latent variables to explain their endogenous counterparts. In this study religiosity and knowledge about COVID-19 vaccines explained a significant proportion of the variance in intention to receive COVID-19 vaccination, R2 = .52. Furthermore, religiosity significantly influenced intention to receive the COVID-19 vaccine, f2 = .17. The effect sizes for knowledge about COVID-19 vaccines and the interaction term of religiosity × knowledge about COVID-19 vaccines were .059 and .078, respectively. Additionally, the model’s predictive relevance (Q2) for religiosity and desire to vaccinate against COVID-19 was greater than 0.
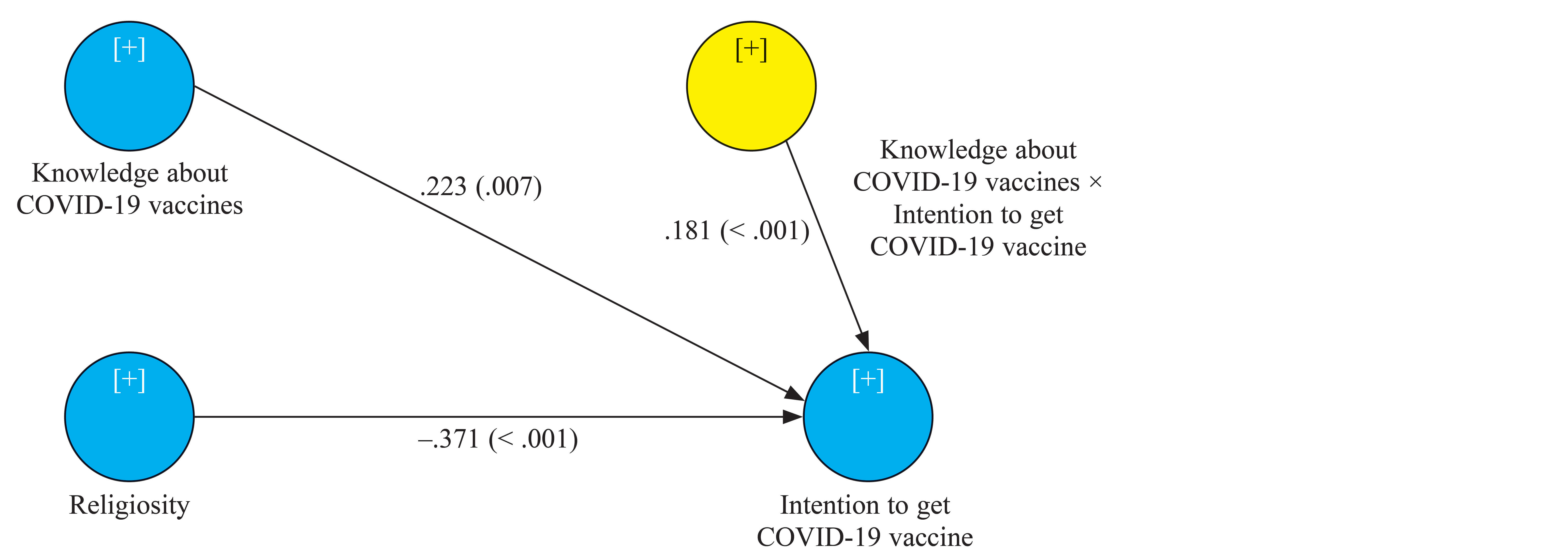
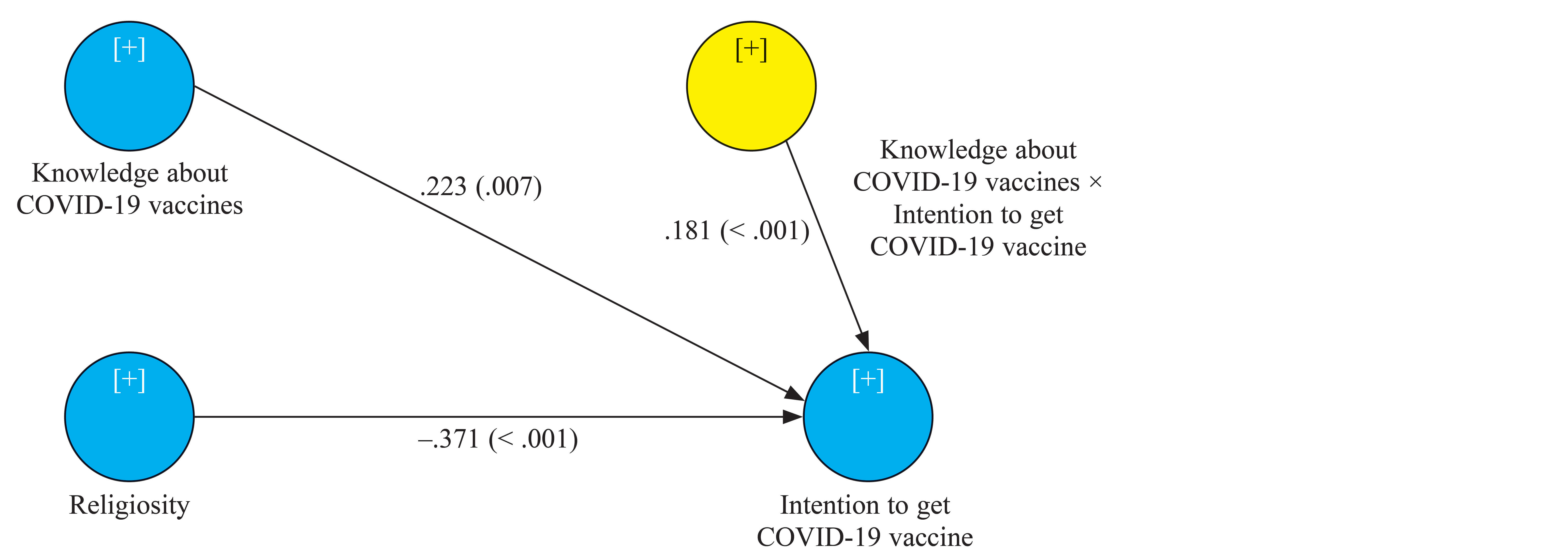
We utilized bootstrapping with 5,000 resamples to test the hypotheses. The findings in Table 2 and Figure 2 indicate that the path coefficient between religiosity and intention to receive the COVID-19 vaccination was significantly negative, β = −.371, t = 5.742, p < .05, providing support for Hypothesis 1. In addition, a significantly positive relationship was observed between knowledge of the COVID-19 vaccine and intention to get vaccinated, β = .223, t = 2.713, p < .05, providing support for Hypothesis 2.
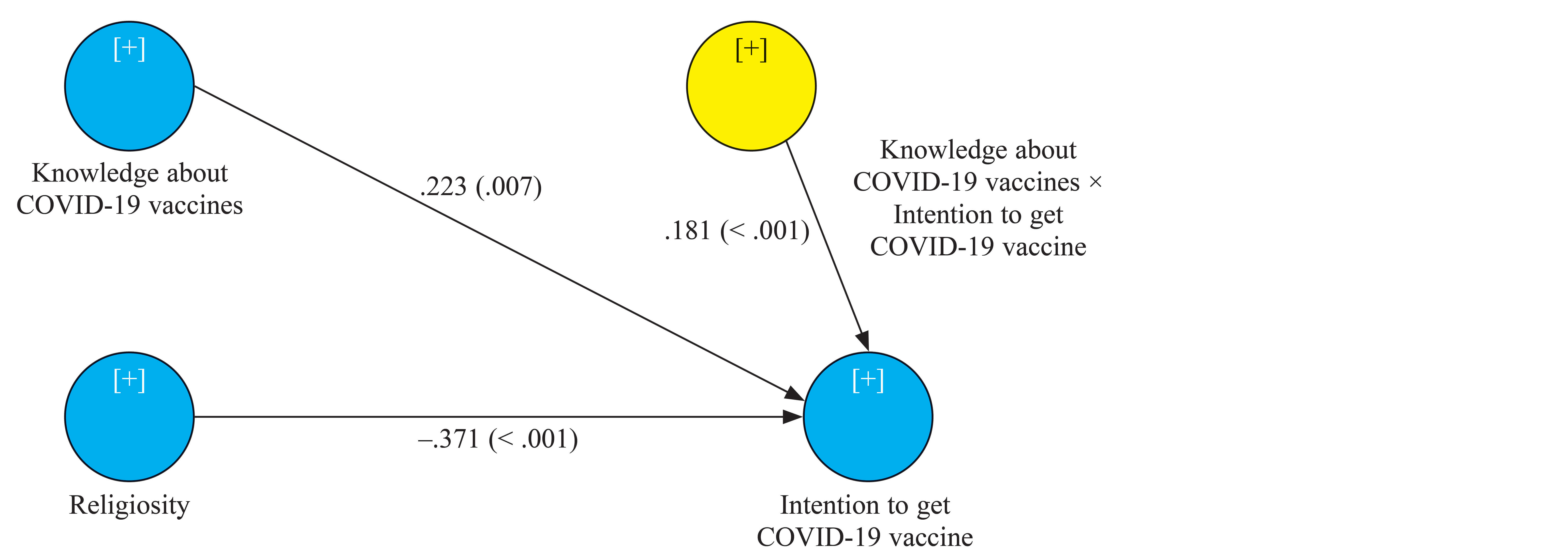
Figure 2. Structural Equation Modeling Results
Note. The numbers shown are path coefficients; p values are shown in parentheses.
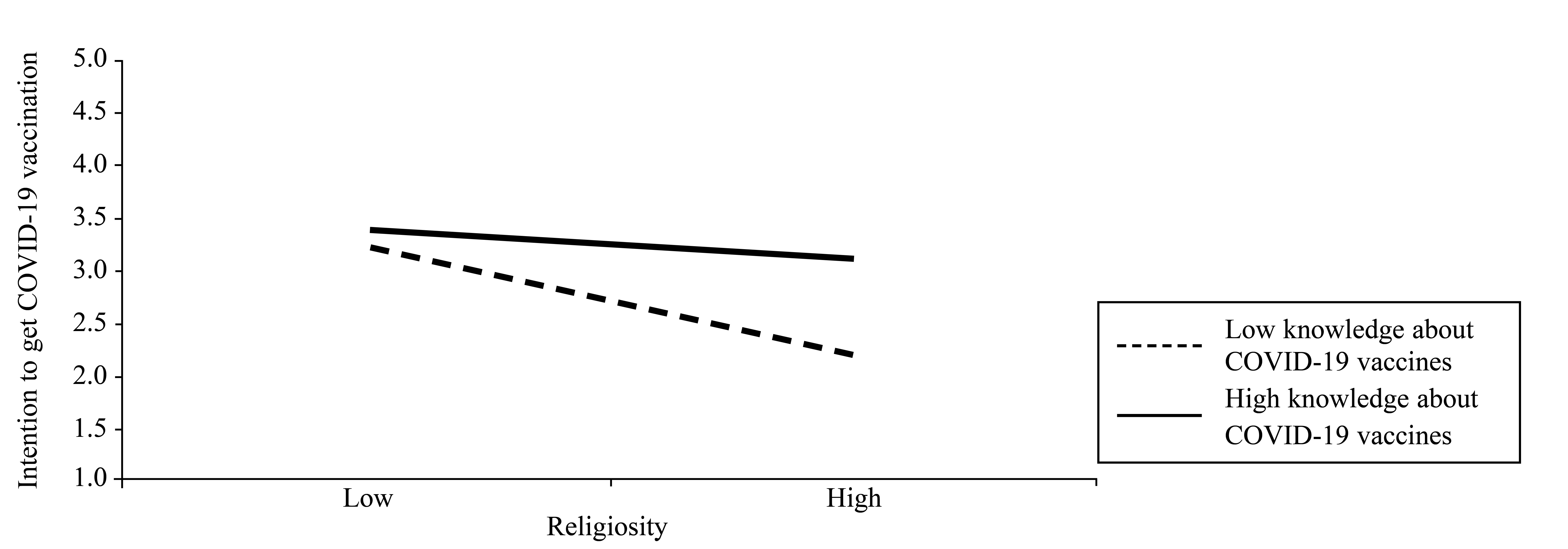
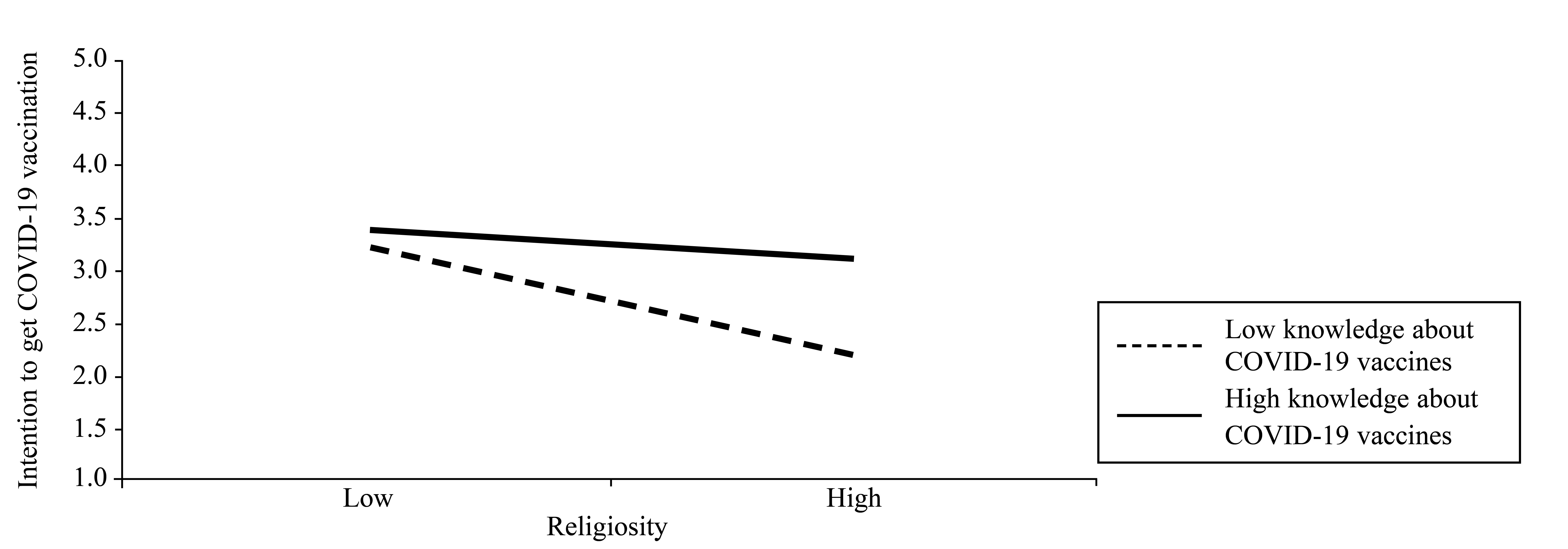
Furthermore, we used 5,000 bootstrapped resamples to generate bias-corrected 95% confidence intervals to estimate the magnitude of the moderation effect. According to the index of moderation (see Figure 3), knowledge of the COVID-19 vaccine substantially moderated the influence of religiosity on COVID-19 vaccination intention, β = .181, t = 3.319, p < .05, indicating that Hypothesis 3 was supported.
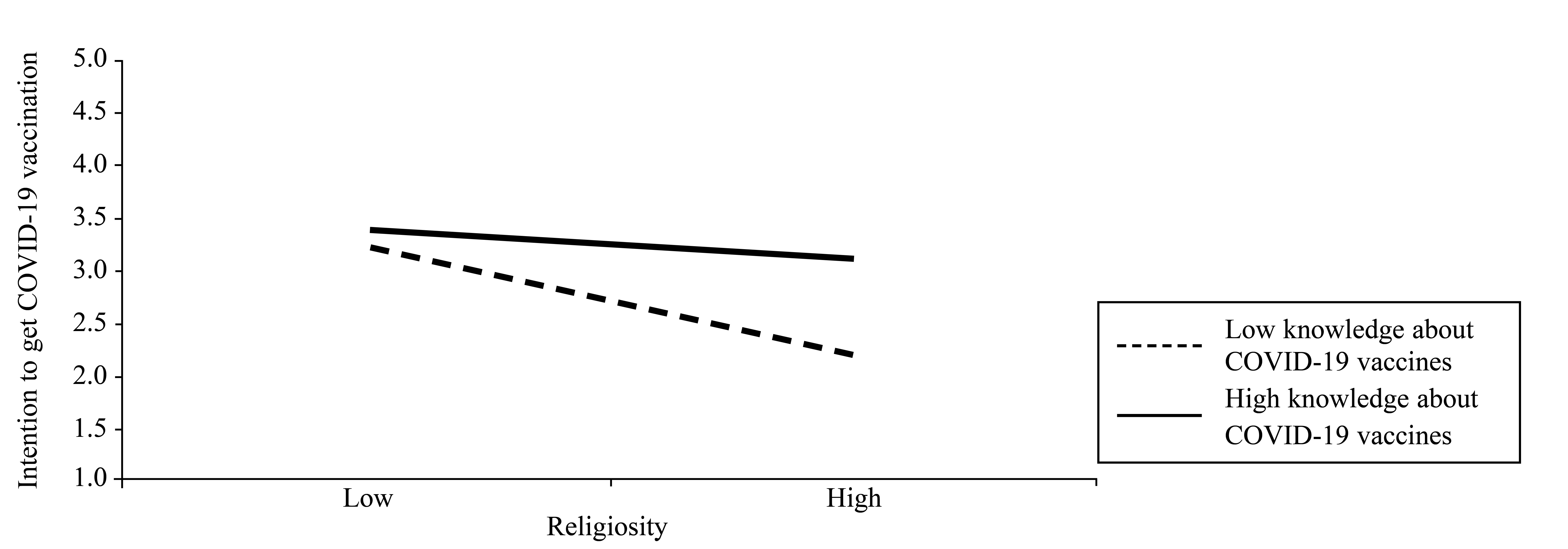
Figure 3. Moderation Analysis
Discussion
This study examined the impact of religiosity and knowledge about the COVID-19 vaccine on individuals’ intention to receive the vaccine. We also investigated how knowledge about COVID-19 vaccines moderated the relationship between religiosity and vaccination intention. The results indicate that religiosity has a negative effect on the willingness of individuals to receive the COVID-19 vaccine. This finding is consistent with previous research indicating that individuals with strong religious beliefs are less likely to accept vaccination (Garcia & Yap, 2021; Jacobi & Vaidyanathan, 2021). Additionally, the study found that people who have a better understanding of the benefits and drawbacks of the COVID-19 vaccine are more willing to receive it (Tegegne et al., 2022). Previous research has shown that educated individuals who are informed about the dangers and benefits of the vaccine are more likely to adopt it (Mohamed et al., 2021; Hossain et al., 2021). Moreover, this study reveals that knowledge about the COVID-19 vaccine reduces the impact of religiosity on vaccine intention. This finding implies that people with vaccine knowledge are more likely to prioritize scientific evidence over religious beliefs when receiving the vaccine. In contrast, people with less knowledge about the vaccine may reject scientific data in favor of religious beliefs. Therefore, raising awareness and knowledge about the COVID-19 vaccine is necessary to encourage vaccine adoption.
Practical Implications
While the scientific discovery of the COVID-19 vaccine is a significant milestone in the fight against the pandemic, this study suggests that people’s faith in religion, rather than scientific evidence, poses an obstacle to vaccine acceptance. To address this, governments and health experts should increase public awareness and promote the importance of the COVID-19 vaccination. This could include launching a campaign among religious experts to emphasize the need for vaccination, and tasking religious scholars with emphasizing the necessity of the vaccine in their daily sermons.
One significant contribution of this study is the finding that knowledge about the COVID-19 vaccine moderates the negative impact of religiosity on the intention to get vaccinated. This highlights the importance of considering both religious beliefs and vaccine knowledge in promoting vaccine acceptance. Evidence suggests that people with knowledge about vaccines have positive beliefs about them and are more likely to get vaccinated. Therefore, it is critical to raise public awareness and knowledge about the COVID-19 vaccine to mitigate the impact of religiosity on vaccination and foster long-term public trust in vaccines. Policymakers and health professionals could take a multisectoral approach, involving various stakeholders such as religious groups, educators, private companies, governments, and other agencies, in promoting vaccine acceptance. By doing so, governments may be able to increase the vaccine acceptance rate among the population.
Limitations and Future Research Directions
This study has some limitations. First, the cross-sectional nature of the study limits interpretation of causality. Second, the respondents were all students; therefore, the findings may not be generalizable to other groups. Future researchers are encouraged to test our research model with diverse groups of people and to collect longitudinal data.
References
Ahmad Kamboh, S., Ittefaq, M., & Sahi, A. A. (2022). Journalistic routines as factors promoting COVID-19 vaccine hesitancy in Pakistan. Third World Quarterly, 43(1), 278–287.
Bok, S., Martin, D. E., & Lee, M. (2021). Validation of the COVID-19 Disbelief Scale: Conditional indirect effects of religiosity and COVID-19 fear on intent to vaccinate. Acta Psychologica, 219, Article 103382.
Brandstetter, S., Böhmer, M. M., Pawellek, M., Seelbach-Göbel, B., Melter, M., Kabesch, M., … KUNO-Kids Study Group. (2021). Parents’ intention to get vaccinated and to have their child vaccinated against COVID-19: Cross-sectional analyses using data from the KUNO-Kids health study. European Journal of Pediatrics, 180(11), 3405–3410.
Dein, S., Loewenthal, K., Lewis, C. A., & Pargament, K. I. (2020). COVID-19, mental health and religion: An agenda for future research. Mental Health, Religion & Culture, 23(1), 1–9.
Dhama, K., Sharun, K., Tiwari, R., Dhawan, M., Bin Emran, T., Rabaan, A. A., & Alhumaid, S. (2021). COVID-19 vaccine hesitancy – Reasons and solutions to achieve a successful global vaccination campaign to tackle the ongoing pandemic. Human Vaccines & Immunotherapeutics, 17(10), 3495–3499.
Garcia, L. L., & Yap, J. F. C. (2021). The role of religiosity in COVID-19 vaccine hesitancy. Journal of Public Health, 43(3), Article e529–e530.
Grabenstein, J. D. (2013). What the world’s religions teach, applied to vaccines and immune globulins. Vaccine, 31(16), 2011–2023.
Hair, J. F., Jr., Hult, G. T. M., Ringle, C. M., & Sarstedt, M. (2022). A primer on partial least squares structural equation modeling (PLS-SEM) (3rd ed.). Sage Publications.
Hamdan, M. B., Singh, S., Polavarapu, M., Jordan, T. R., & Melhem, N. M. (2021). COVID-19 vaccine hesitancy among university students in Lebanon. Epidemiology & Infection, 149, Article 242.
Henseler, J., Ringle, C. M., & Sarstedt, M. (2015). A new criterion for assessing discriminant validity in variance-based structural equation modeling. Journal of the Academy of Marketing Science, 43, 115–135.
Hossain, E., Rana, J., Islam, S., Khan, A., Chakrobortty, S., Ema, N. S., & Bekun, F. V. (2021). COVID-19 vaccine-taking hesitancy among Bangladeshi people: Knowledge, perceptions and attitude perspective. Human Vaccines & Immunotherapeutics, 17(11), 4028–4037.
Jacobi, C. J., & Vaidyanathan, B. (2021). Racial differences in anticipated COVID-19 vaccine acceptance among religious populations in the US. Vaccine, 39(43), 6351–6355.
Kasri, R. A., Ahsan, A., Widiatmoko, D., & Hati, S. R. H. (2023). Intention to consume halal pharmaceutical products: Evidence from Indonesia. Journal of Islamic Marketing, 14(3), 735–756.
Kock, N. (2015). Common method bias in PLS-SEM: A full collinearity assessment approach. International Journal of e-Collaboration, 11(4), 1–10.
Lazarus, J. V., Ratzan, S. C., Palayew, A., Gostin, L. O., Larson, H. J., Rabin, K., … El-Mohandes, A. (2021). A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine, 27(2), 225–228.
Li, W. W., Miller, D., Shapiro, S., & Narayanan, A. (2023). Mindfulness and mental health in the time of the COVID-19 pandemic. Frontiers in Psychology, 14, Article 1209911.
Mohamed, N. A., Solehan, H. M., Mohd Rani, M. D., Ithnin, M., & Che Isahak, C. I. (2021). Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: A web-based survey. PLoS ONE, 16(8), Article e0256110.
Tegegne, M. D., Girma, S., Mengistu, S., Mesfin, T., Adugna, T., Kokeb, M., … Wubante, S. M. (2022). Willingness to receive COVID-19 vaccine and associated factors among adult chronic patients. A cross-sectional study in Northwest Ethiopia. PLoS ONE, 17(7), Article e0269942.
Trepanowski, R., & Drążkowski, D. (2022). Cross-national comparison of religion as a predictor of COVID-19 vaccination rates. Journal of Religion and Health, 61(3), 2198–2211.
Wang, Y.-C., Chi, C. G.-Q., & Erkılıç, E. (2021). The impact of religiosity on political skill: Evidence from Muslim hotel employees in Turkey. International Journal of Contemporary Hospitality Management, 33(3), 1059–1079.
Wong, L. P., Alias, H., Wong, P.-F., Lee, H. Y., & AbuBakar, S. (2020). The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Human Vaccines & Immunotherapeutics, 16(9), 2204–2214.
Zheng, H., Jiang, S., & Wu, Q. (2022). Factors influencing COVID-19 vaccination intention: The roles of vaccine knowledge, vaccine risk perception, and doctor-patient communication. Patient Education and Counseling, 105(2), 277–283.
Ahmad Kamboh, S., Ittefaq, M., & Sahi, A. A. (2022). Journalistic routines as factors promoting COVID-19 vaccine hesitancy in Pakistan. Third World Quarterly, 43(1), 278–287.
Bok, S., Martin, D. E., & Lee, M. (2021). Validation of the COVID-19 Disbelief Scale: Conditional indirect effects of religiosity and COVID-19 fear on intent to vaccinate. Acta Psychologica, 219, Article 103382.
Brandstetter, S., Böhmer, M. M., Pawellek, M., Seelbach-Göbel, B., Melter, M., Kabesch, M., … KUNO-Kids Study Group. (2021). Parents’ intention to get vaccinated and to have their child vaccinated against COVID-19: Cross-sectional analyses using data from the KUNO-Kids health study. European Journal of Pediatrics, 180(11), 3405–3410.
Dein, S., Loewenthal, K., Lewis, C. A., & Pargament, K. I. (2020). COVID-19, mental health and religion: An agenda for future research. Mental Health, Religion & Culture, 23(1), 1–9.
Dhama, K., Sharun, K., Tiwari, R., Dhawan, M., Bin Emran, T., Rabaan, A. A., & Alhumaid, S. (2021). COVID-19 vaccine hesitancy – Reasons and solutions to achieve a successful global vaccination campaign to tackle the ongoing pandemic. Human Vaccines & Immunotherapeutics, 17(10), 3495–3499.
Garcia, L. L., & Yap, J. F. C. (2021). The role of religiosity in COVID-19 vaccine hesitancy. Journal of Public Health, 43(3), Article e529–e530.
Grabenstein, J. D. (2013). What the world’s religions teach, applied to vaccines and immune globulins. Vaccine, 31(16), 2011–2023.
Hair, J. F., Jr., Hult, G. T. M., Ringle, C. M., & Sarstedt, M. (2022). A primer on partial least squares structural equation modeling (PLS-SEM) (3rd ed.). Sage Publications.
Hamdan, M. B., Singh, S., Polavarapu, M., Jordan, T. R., & Melhem, N. M. (2021). COVID-19 vaccine hesitancy among university students in Lebanon. Epidemiology & Infection, 149, Article 242.
Henseler, J., Ringle, C. M., & Sarstedt, M. (2015). A new criterion for assessing discriminant validity in variance-based structural equation modeling. Journal of the Academy of Marketing Science, 43, 115–135.
Hossain, E., Rana, J., Islam, S., Khan, A., Chakrobortty, S., Ema, N. S., & Bekun, F. V. (2021). COVID-19 vaccine-taking hesitancy among Bangladeshi people: Knowledge, perceptions and attitude perspective. Human Vaccines & Immunotherapeutics, 17(11), 4028–4037.
Jacobi, C. J., & Vaidyanathan, B. (2021). Racial differences in anticipated COVID-19 vaccine acceptance among religious populations in the US. Vaccine, 39(43), 6351–6355.
Kasri, R. A., Ahsan, A., Widiatmoko, D., & Hati, S. R. H. (2023). Intention to consume halal pharmaceutical products: Evidence from Indonesia. Journal of Islamic Marketing, 14(3), 735–756.
Kock, N. (2015). Common method bias in PLS-SEM: A full collinearity assessment approach. International Journal of e-Collaboration, 11(4), 1–10.
Lazarus, J. V., Ratzan, S. C., Palayew, A., Gostin, L. O., Larson, H. J., Rabin, K., … El-Mohandes, A. (2021). A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine, 27(2), 225–228.
Li, W. W., Miller, D., Shapiro, S., & Narayanan, A. (2023). Mindfulness and mental health in the time of the COVID-19 pandemic. Frontiers in Psychology, 14, Article 1209911.
Mohamed, N. A., Solehan, H. M., Mohd Rani, M. D., Ithnin, M., & Che Isahak, C. I. (2021). Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: A web-based survey. PLoS ONE, 16(8), Article e0256110.
Tegegne, M. D., Girma, S., Mengistu, S., Mesfin, T., Adugna, T., Kokeb, M., … Wubante, S. M. (2022). Willingness to receive COVID-19 vaccine and associated factors among adult chronic patients. A cross-sectional study in Northwest Ethiopia. PLoS ONE, 17(7), Article e0269942.
Trepanowski, R., & Drążkowski, D. (2022). Cross-national comparison of religion as a predictor of COVID-19 vaccination rates. Journal of Religion and Health, 61(3), 2198–2211.
Wang, Y.-C., Chi, C. G.-Q., & Erkılıç, E. (2021). The impact of religiosity on political skill: Evidence from Muslim hotel employees in Turkey. International Journal of Contemporary Hospitality Management, 33(3), 1059–1079.
Wong, L. P., Alias, H., Wong, P.-F., Lee, H. Y., & AbuBakar, S. (2020). The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Human Vaccines & Immunotherapeutics, 16(9), 2204–2214.
Zheng, H., Jiang, S., & Wu, Q. (2022). Factors influencing COVID-19 vaccination intention: The roles of vaccine knowledge, vaccine risk perception, and doctor-patient communication. Patient Education and Counseling, 105(2), 277–283.